40 YEAR MALE WITH COMPLAINTS OF BOUTS OF VOMITINGS
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
Ihave been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 40 years male, resident of chityala, field assistant by occupation came to the opd with chief complaints of vomitings 2 days back
History of presenting illness:
Patient was apparently asymptomatic 2 days back and then he started developing vomitings ( 18 episodes till yesterday )
Non bilious, non projectile, non blood stained in nature with watery consistency and is associated with squeezing feeling in the epigastrium region each time preceeding the vomiting episode.
No history of associated symptoms like fever, diarrhoea, chest pain, abdominal pain, abdominal distension, constipation, headache, giddiness.
Past history:
History of diabetic ulcer on the heel since 2 months( healing) and on great toe since 1 month.
History of diabetes mellitus since 6 months( on medication)and hypertension since 2 months( not on medication).
No history of asthma,CAD,Tuberculosis and epilepsy.
Treatment history:
Patient was on metformin 500mg since 6 months.
Family history:
History of diabetes mellitus in mother since 15 years and elder brother since 10 years.
Personal history:
Diet: mixed
Appetite: normal
Sleep: Adequate but interrupted during nights when he gets up to micturate
Bowel movements: normal
Bladder movements: Interrupted urine flow
Addictions: Alcohol 180ml per day for 10 years and then stopped since 2 months.
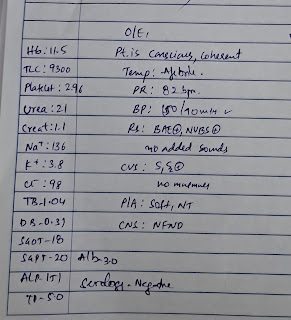
General examination:
Patient is conscious coherent and cooperative
Moderately built and Moderately nourished
Vitals:
Pulse: 72 bpm
RR: 16cpm
Bp: 120/80 mm Hg
Temp: Afebrile
No pallor, icterus,cyanosis,koilonychia, clubbing, generalised lymphadenopathy, pedal edema
Systemic examination:
CVS : S1 S2 heard. No thrills and murmurs
CNS: No focal neurological deficit.
RS: Bilateral air entry present.
Normal vesicular breath sounds
Abdomen:
Shape: scaphoid
Soft, nontender, no organomegaly
Bowel sounds: Normal
Genitals: Normal
Provisional diagnosis
Gastritis?
Food piosioning?
Diabetic foot?
Treatment:
Day1
Inj.PANTOPREZOLE 40 mg
Inj.ZOFER 4mg
Inj.METOCLOPROMIDE iv stat
Day2
Tab METFORMIN 500mg
Tab GLIMIPERIDE 1mg




Comments
Post a Comment